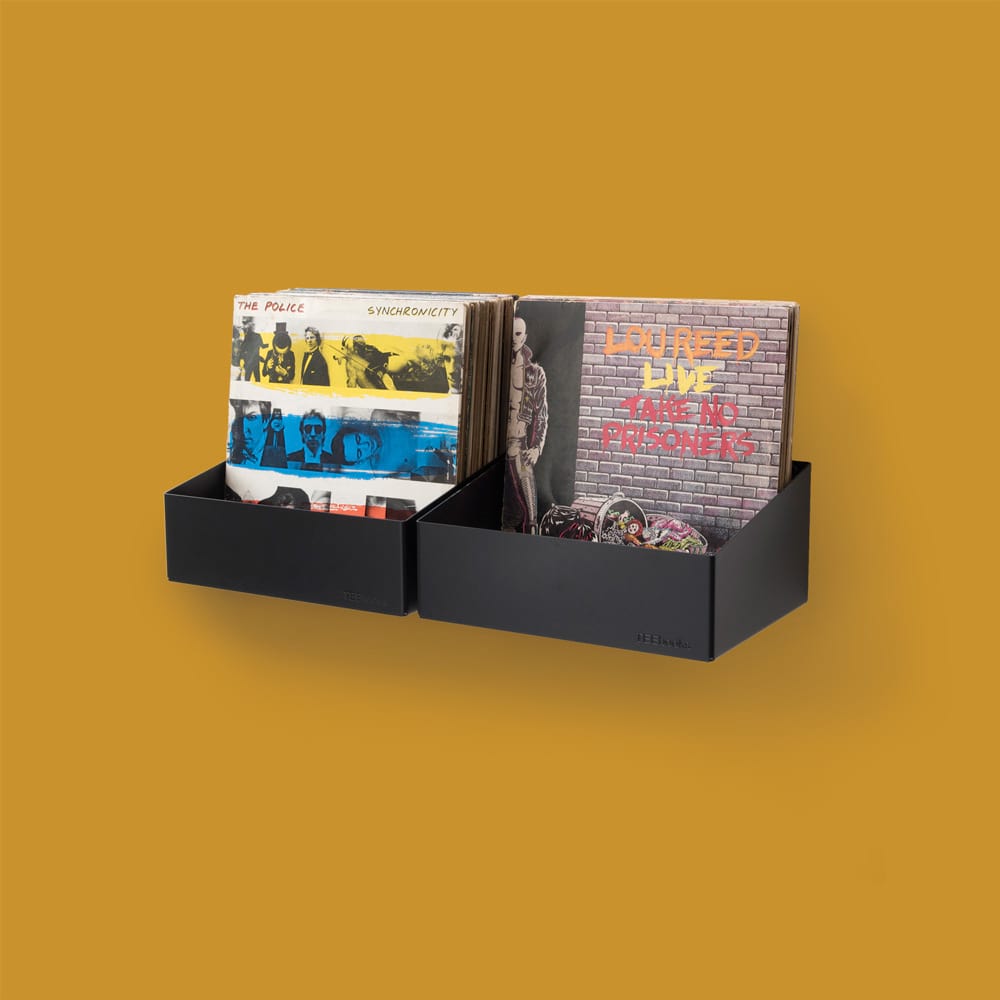
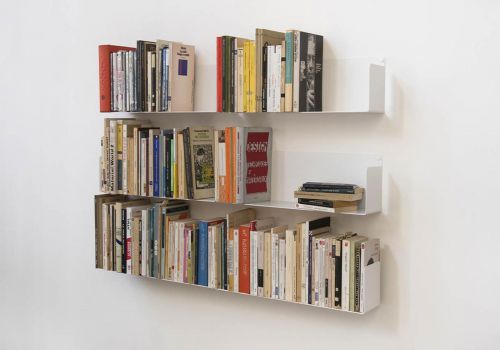
Étagère design by TEEbooks
Notre sélection d'étagères
Voir tous
-
 Prix 46,80 € Prix normal 78,00 € -31,20 €
Prix 46,80 € Prix normal 78,00 € -31,20 €- Nouveauté !
- -40 %
-
 Prix 98,00 € Prix normal 118,00 € -20,00 €
Prix 98,00 € Prix normal 118,00 € -20,00 €- Nouveauté !
- -16 %
-
 Prix 229,00 € Prix normal 260,00 € -31,00 €
Prix 229,00 € Prix normal 260,00 € -31,00 €- Prix en baisse
- -11 %
-
- Prix en baisse
- -9 %
-

- Prix en baisse
- -13 %
-
 Prix 332,00 € Prix normal 390,00 € -58,00 €
Prix 332,00 € Prix normal 390,00 € -58,00 €- Prix en baisse
- -14 %
-

- Prix en baisse
- -15 %
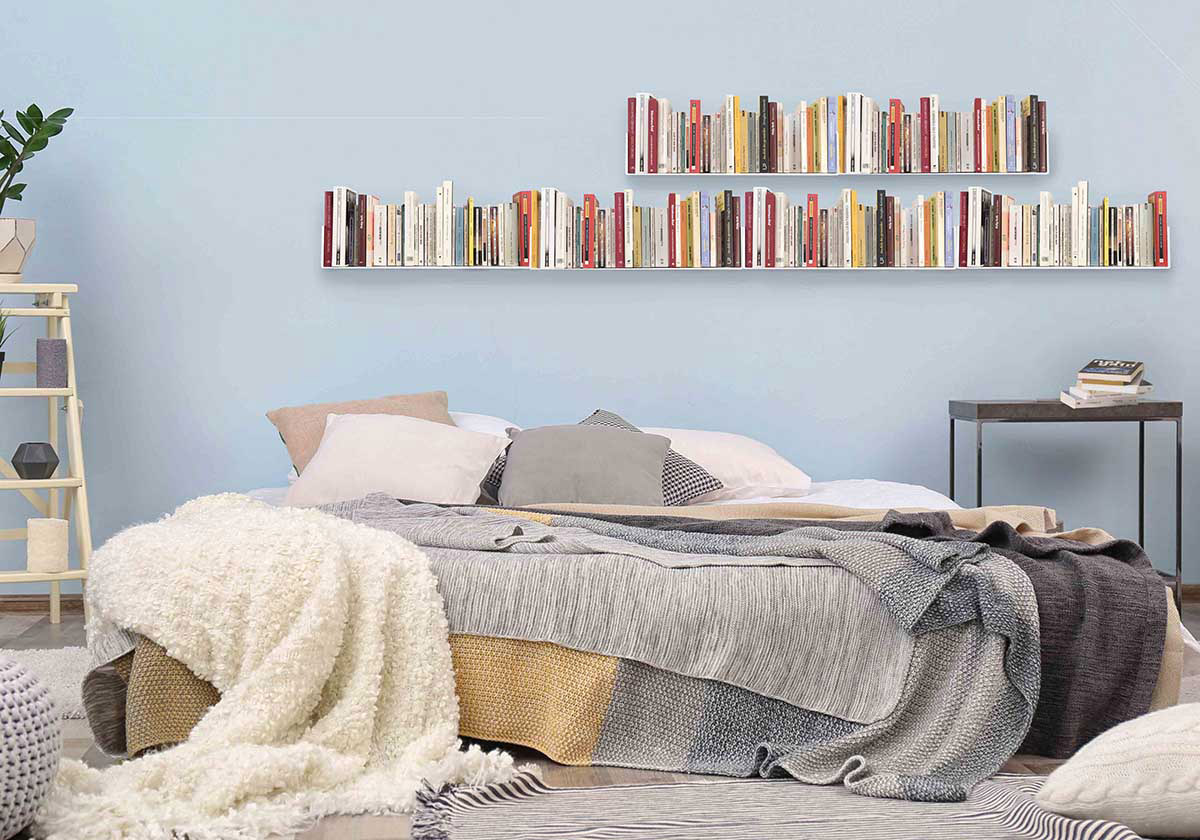
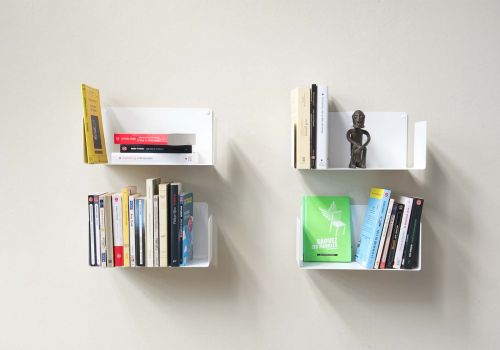
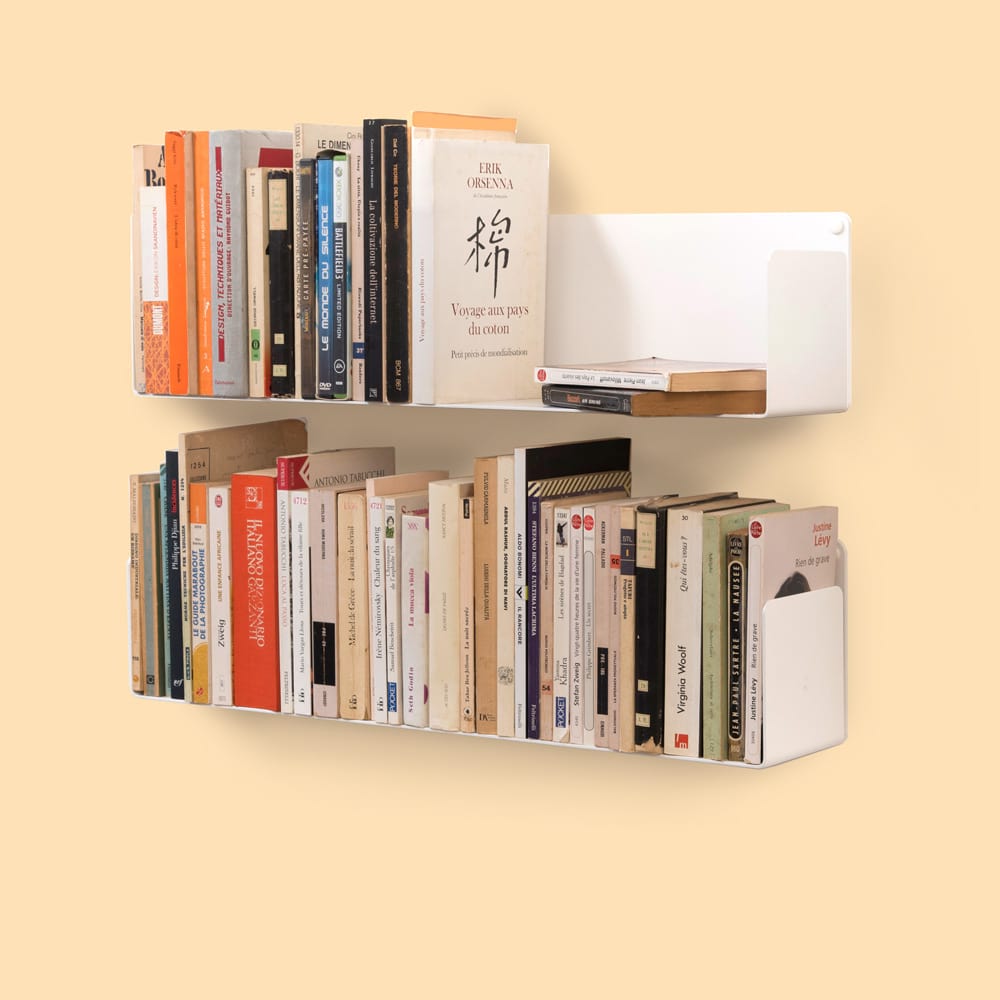
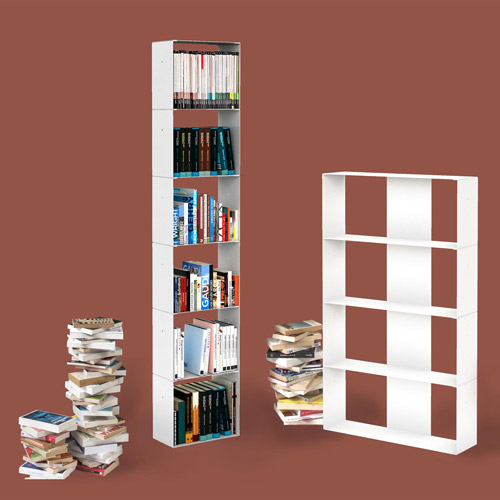
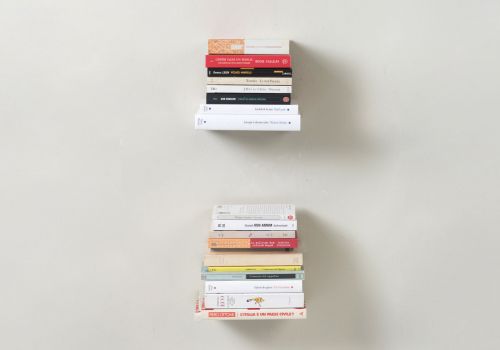
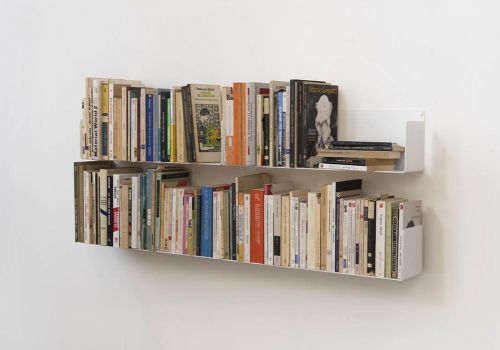
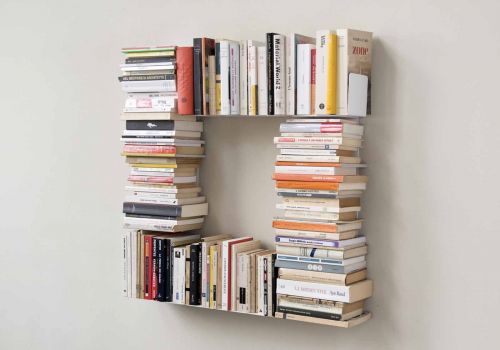
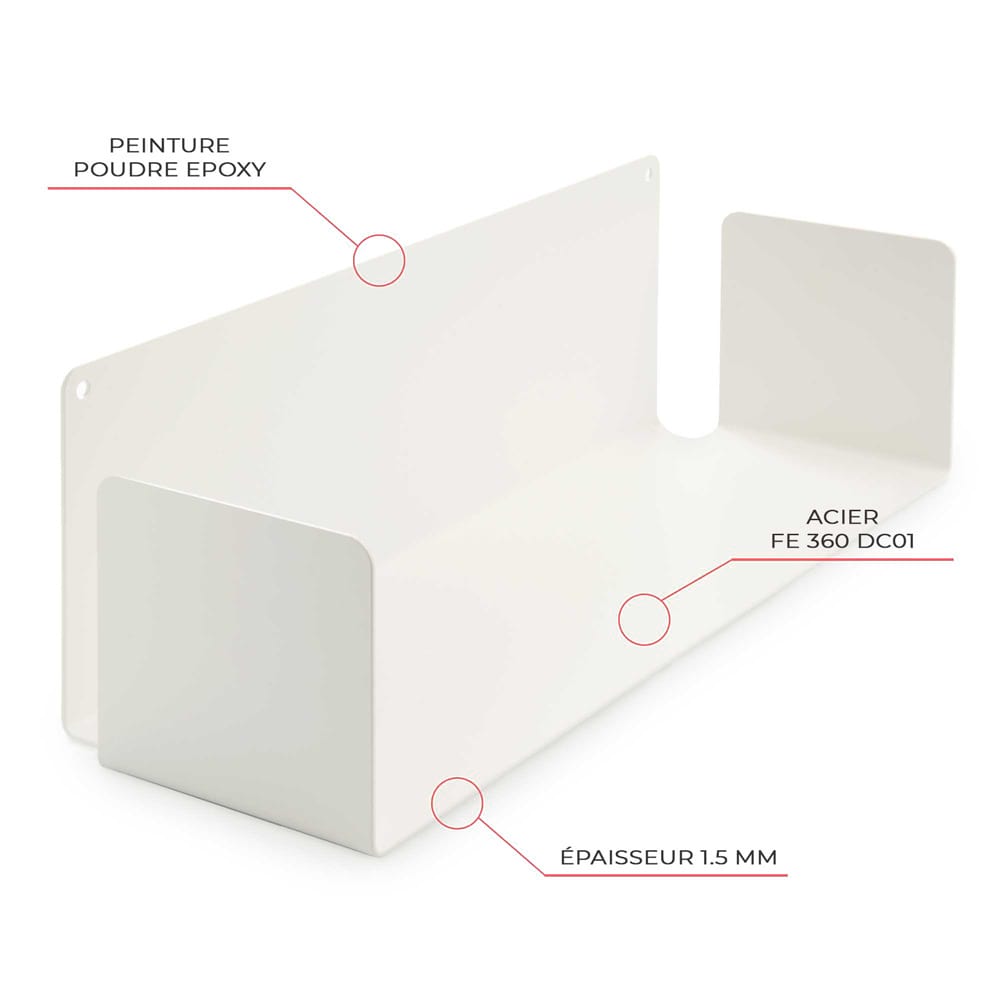
Simple, Utile et Design
Nos étagères s'adaptent à tous vos styles d'intérieur
Découvrez nos étagères
Trouvez votre inspiration